There have been a number of questions on the Johns Hopkins pancreatic website regarding stereotactic radiosurgery for pancreatic cancer. Therefore, we thought it is important to review the literature on stereotactic radiosurgery and help patients better understand the risks and benefits of this treatment and clarify some of the misconceptions. Stereotactic radiosurgery (SRS) can also be called stereotactic body radiotherapy (SBRT) or CyberKnife. It is important to stress that all of these modalities use radiation and that there is no actual surgery done.
The theory is that the radiation doses are high enough to cause ablation of the pancreatic tumor. While the data suggests that SBRT and/or CyberKnife can ablate certain tumors (brain metastasis and lung tumors) there is no prospective data showing that SBRT and/or CyberKnife can effectively ablate pancreatic tumors or shrink them to the point where they can be resectable. As you can see by the two prospective trials posted on this blog, SBRT and CyberKnife appear to prevent pancreatic tumors from progressing (grow) but there is no evidence that it causes pancreatic tumors to shrink or improve survival. Further, the data suggests that high doses of radiation given by SBRT or CyberKnife can cause some unacceptable acute (within 2-3 months of treatment) and chronic side effects from treatment when compared to conventional radiation treatment delivered over 2-6 weeks of treatment. Specifically, approximately 30-40% of all patients treated with SBRT/CyberKnife develop gastrointestinal side effects including a small number of patients who developed ulcers which required surgical repair. The authors suggest that this may be because the duodenum and small bowel is adjacent to the pancreatic tumors and it is hard to treat the pancreatic tumor and avoid irradiating these areas.
It is important that almost all patients in these studies developed metastatic disease, clearly demonstrating a need for better drugs to control pancreatic tumor spread. Finally, the survival in both of these studies unfortunately were very similar to conventional radiation and chemotherapy. While SBRT and CyberKnife are more convenient for patients (1-5 days of treatment) compared with 25 treatments (conventional), the increased risk of side effects with shorter course radiation with no improved survival make us question whether these treatments in their CURRENT FORM are clearly benefiting patients with pancreatic cancer.
It is important to note that the doses of radiation used in these studies are high. In the Stanford CyberKnife study (Koong et al.) the dose was 25 Gy given in one fraction and in the SBRT (Denmark) trial the total dose was 45 Gy. It is possible that lower doses (15-25) delivered over 3-5 fractions may be better tolerated than the doses given in these two studies, however this data has not been published in a prospective controlled fashion. In summary, SBRT/CyberKnife does appear to result in good local control of pancreatic tumors, however it is unlikely that it will shrink a majority of pancreatic tumors enough for surgical resection and patients are likely to have increased chronic (long term) side effects when compared to conventional treatment.
Additional prospective (patients treated on a clinical trial and followed for side effects) studies are needed to test the true benefit and safety of SBRT and Cyberknife treatment for patients with unresectable pancreatic cancer. While SBRT and CyberKnife therapy does hold promise we have to be careful not to tell patients that it is likely to cure them of their cancer….the data simply isn’t there.
Commonly asked questions:
1) What is CyberKnife and how does it differ from stereotactic body radiation therapy (SBRT)? How does it differ from standard conventional radiation?
a. Cyberknife and SBRT are both radiation. No surgery is actually done. The theory is that high doses of radiation (15-45 Gy) given over a shorter period of time (1-5 days) can more effectively kill pancreatic cancer cells when compared to conventional radiation (50 Gy) given over a 5 week period. CyberKnife and SBRT are both attractive because they limit the amount of time a patient needs to undergo radiation (1 week vs. 5 weeks). While higher doses of radiation may more effectively kill pancreatic cancer cells, it can also cause more damage to normal tissues which are directly adjacent to the pancreas tumor such as the duodenum or bowel.
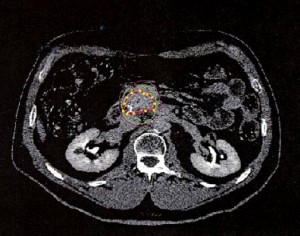
b. CyberKnife can deliver beams from 1200 or more different directions, a capability that allows it to target lesions precisely. Often 100 beams of radiation are used in each treatment plan. Using multiple beams of radiation can limit the dose to adjacent structures. The treatment is also non-isocentric which means it does not rely on one point in the tumor and can deliver beams of radiation to any area of the tumor. It relies on a robotic arm to track gold seed markers in the tumor which can move during breathing. Treatment time can be 1-2 hours. One limitation is the beams of radiation are not able to treat the patient from all directions (360 degrees) and sometimes the patient needs to be turned over during radiation treatment.
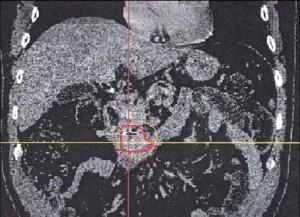
c. SBRT uses 10-25 beams of radiation. It also can limit adjacent structures. The treatment is isocentric meaning it relies on a central spot in the tumor to focus the radiation. Often gold seed markers are used to track the tumor. The machine can deliver radiation all around the body (360 degrees). Rather than using a robotic arm to track the tumor, SBRT tries to control or limit breathing motion with specific body molds or breathing devices (airway, breathing, control devices-ABC). The treatment time is typically 20-40 mintues. There have been no real head-to-head comparisons of CyberKnife and SBRT in the treatment of pancreatic cancer. However, in other sites they have been shown to have comparable results (lung cancer).
2) Does SBRT/CyberKnife cure patients of pancreatic cancer and/or improve survival? Although there may be anecdotal evidence of this, there is no published data showing that SBRT/CyberKnife cures patients of pancreatic cancer. There is no evidence to show that CyberKnife clearly improves survival compared to conventional chemotherapy and radiation.
3) Does SBRT/CyberKnife improve local control? Based on CT and PET/CT imaging, higher doses of radiation does appear to improve local control compared to conventional radiation however in its current form (15-45 Gy delivered in 1-5 fractions) it does appear to cause more chronic side effects (gastrointestinal) when compared to conventional treatment.
4) Should I be treated with CyberKnife? While SBRT/CyberKnife is promising, additional prospective studies are needed to determine the optimal daily and total dose of radiation needed to improve local control while limiting treatment related side effects. Patients should be consulted by a radiation oncologists who has ample experience in the treatment of patients with CyberKnife and SBRT.
5) Does Johns Hopkins have SBRT/CyberKnife? Johns Hopkins does not have CyberKnife, however we do have SBRT. We are currently writing a protocol to determine the optimal dose for SBRT with several other institutions and we hope to be enrolling patients on this trial in the next year. Currently we use a short course (2 weeks) of radiation or conventional radiation (5 weeks) with chemotherapy which does downstage a small proportion of patients with limited side effects (10-15%).
For more information on the studies discussed in this blog please click below:
Cyberknife Pancreas PDF (Koong et al.)
Stereotactic Radiation Pancreas PDF (Hoyer et al.)
Please feel free to email me with any questions or comments.