Significant progress has been made over the past two decades on the pathogenesis of individual neurodegenerative diseases, including Alzheimer’s disease (AD), amyotrophic lateral sclerosis (ALS) and frontotemporal dementia (FTD). However, different neurodegenerative syndromes have been mainly studied mechanistically in isolation. There has been a lack of concerted effort to ascertain whether and how these pathogenic processes may be linked to one another. In the most recent issue of journal Acta Neuropathologica, Dr. Mingkuan Sun, William Bell and Katherine LaClair, co-first authored a report about cryptic exon incorporation in Alzheimer’s disease cases exhibiting TDP-43 pathology. This is the first evidence on how loss of TDP-43 function from neurons, a common shared feature with ALS and FTD, could contribute to pathogenesis of AD.
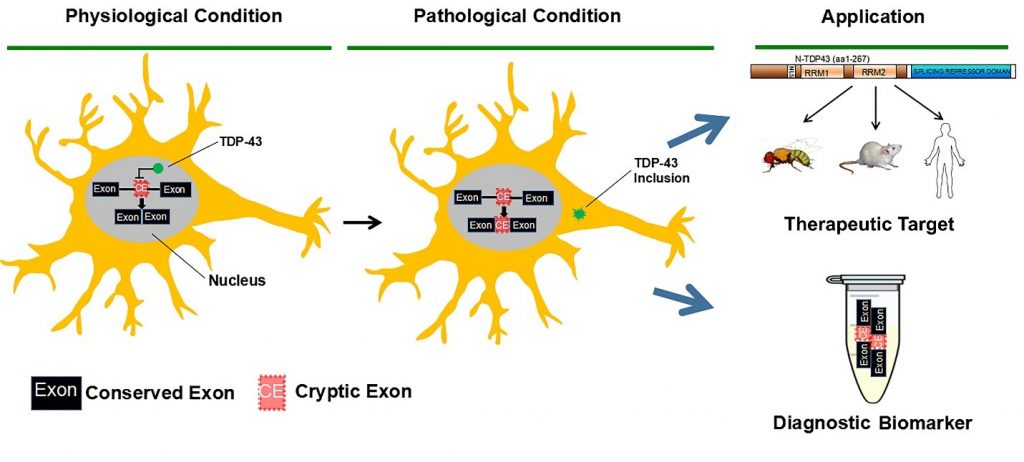
It has been known for years that other factors besides Aβ and tau also contribute to neurodegeneration and cognitive failure in AD. The most convincing evidence is that 20-40% of cognitively normal older individuals have levels of Aβ and tau pathology that are indistinguishable from patients with severe clinical symptoms of AD. Recent work showed that non-canonical pathologies occur in up to 75% of AD cases, including TDP-43 proteinopathy, α-synuclein “Lewy bodies”, and tau “Pick bodies” that are associated with neurodegeneration in separately classified diseases. TDP-43 proteinopathy is characterized by cytoplasmic aggregation of the transactivation response element DNA-binding protein 43 (TDP-43) accompanied by its nuclear clearance, and was first identified in another neurodegenerative disease spectrum, ALS-FTD. Identified as an essential gene, TDP-43 is also required for aspects of neuronal physiology in mice, fruit flies and zebrafish. Notably, TDP-43 proteinopathy is one of the most common non-canonical pathologies observed in AD cases and is strongly associated with worsened neurodegeneration and cognition, suggesting a convergent mechanism of neurodegeneration with ALS and FTD.
In their paper, Sun et al. found that cryptic exon incorporation occurred in all AD cases exhibiting TDP-43 pathology. Furthermore, incorporation of cryptic exons was observed in the hippocampus when TDP-43 inclusions was restricted only to the amygdala, the earliest stage of TDP-43 progression. Most importantly, cryptic exon incorporation could be detected in AD brains lacking TDP- 43 inclusions, but exhibiting nuclear clearance of TDP-43. These data support the notion that the functional consequence of nuclear depletion of TDP-43, as determined by cryptic exon incorporation, likely occurs as an early event of TDP-43 proteinopathy and may have greater contribution to the pathogenesis of AD than currently appreciated. This study has opened new direction in AD research as early detection and effective repression of cryptic exons in AD patients may offer important diagnostic and therapeutic implications for this devastating illness of the elderly.
Co-authors were Jonathan Ling, Heather Han, Yusuke Kageyama, Olga Pletnikova, and Juan Troncoso of Johns Hopkins Brain Resource Center. The work was supported in part by the Johns Hopkins Neuropathology Pelda fund and the NIH Grant to Dr. Philip Wong; McKnight Award for Memory and Cognitive Disorder and the Johns Hopkins Alzheimer’s Disease Research Center pilot grant to Dr. Liam Chen.