In search of treatments and cures for diseases like Alzheimer’s and Parkinson’s, researchers need actual human tissue. The Brain Resource Center has the diseased and healthy specimens they’re after.
The article below was originally published in the HUB Magazine.
The brain of Michael W. displayed many of the hallmark characteristics of Alzheimer’s disease. There were visible clumps of beta-amyloid protein fragments wedged between nerve cells. Our chemistry normally breaks down and eliminates these proteins, but with Alzheimer’s the fragments accumulate to form hard, insoluble plaques. Michael’s brain also showed a buildup of tau protein inside some cells, which cause twists and tangles that can lead to cell structure collapse and a breakdown of the communication between neurons.
Over time, the buildup of these proteins goes unabated, and brain cells begin to malfunction. As Alzheimer’s disease progresses, more cells become affected and brain tissue shrinks. In the early stages of AD, short-term memory begins to decline. Then judgment worsens, emotional outbursts may occur, and language is impaired. In the final stages, people may lose the ability to feed themselves, speak, recognize loved ones, and control bodily functions.
But in the case of Michael W., none of this happened.
Michael W. lived to age 90 with no signs of cognitive decline, according to a thorough physical and mental examination that took place just months before his death. His memory remained intact. He might even have played chess and done crosswords right up until his final days.
Something, or perhaps a number of somethings, in Michael W.’s genetic makeup and body chemistry protected him from the ravages of a disease that affects one-third of Americans over age 85 and 44 million people worldwide, and is the sixth-leading cause of death in the United States.
Scientists would love to know why this man, and others like him, was “lucky.”
Not surprisingly, Michael’s brain—actually microthin slices, frozen chunks, and wax-encased blocks of it—is an oft-requested item in the collection of the School of Medicine’s Brain Resource Center, a tissue repository for faculty at JHU and academic centers around the country.
Researchers need human brain tissue to test hypotheses and confirm findings as they seek treatments and cures for diseases that affect millions of people worldwide. The Brain Resource Center specializes in neurological disease cases, specifically Alzheimer’s, Parkinson’s disease, Huntington’s disease, and various dementias. But the collection doesn’t stop there. It also includes relatively healthy brains used as controls, mostly from participants of the Baltimore Longitudinal Study of Aging, which since 1958 has tracked individuals from their 40s until death and is one of the longest-running studies of aging. The center’s long list of clients represents the fields of pathology, imaging, neurology, psychiatry, molecular biology, genetics, neuroscience, and anatomy.
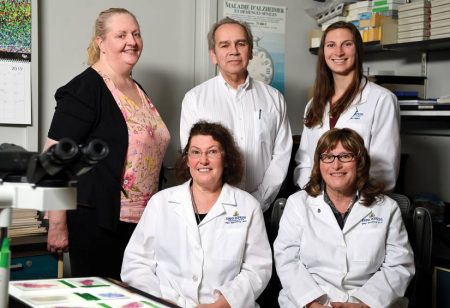
We really are the hub for morphological studies of human brains here at Johns Hopkins,” says Juan Troncoso, the center’s longtime director and a professor of pathology and neurology at the School of Medicine.
And business is good. The center, located in the Ross Research Building at the East Baltimore campus, currently houses pieces of roughly 2,800 brains, which fill just about every available nook and cranny in the multiroomed space. Turn any corner, you will find “wet brains” stacked on top of shelves and inside cabinets. Not whole brains floating in glass jars, as you might see in the movies but rather brain halves bathing in a yellowish formalin solution in plastic containers. And then there are thousands upon thousands of numbered and color-coded histological and diagnostic slides of brain slices that fill metal filing cabinets. Hundreds of larger chunks of brains reside in industrial-size freezers that line the center’s hallways. Brains here, there, and everywhere.
“We need more space,” says Troncoso, sitting in his office and leaning back in his chair one spring afternoon. “The space that we have is somewhat pitiful compared to the productivity that we have. Many of the neurological studies that go on here at Johns Hopkins involve the use of our brains.”

What makes the BRC’s collection so valuable is that nearly every brain comes with a detailed history. Like Michael W., many donors had been Johns Hopkins patients and participants of clinical and long-term studies. In some cases, the BRC has decades of clinical data that document the health of an individual and the steady progression of disease. “We have a thorough cardiovascular and neurological assessment of donors from the BLSA,” he says. “In some cases, every doctor’s visit, every routine check. We can then compare that to what we’re physically seeing in the brain. You can have a tremendous basic science department, but the reason for its existence is to eventually bring some benefit for human disease. But the only way to test a hypothesis is with human material. If you don’t have that, a lot of the basic research won’t have an application. That is why the work we do and this collection are so critical.”
The Johns Hopkins Brain Resource Center was founded in 1979 by Troncoso’s mentor, Donald L. Price, a professor of pathology, neurology, and neuroscience and former director of the Neuropathology Division and the Johns Hopkins Alzheimer’s Disease Research Center. At the time, Alzheimer’s disease study was very much in its infancy, and researchers needed human tissue to help discover what was going wrong with brain function.
The first donated brain was stored in the Johns Hopkins Hospital’s Pathology Building, which effectively became the first brain bank in the United States devoted to Alzheimer’s disease. Over the next decade, the center would branch out and collect the brains of those with Huntington’s, a genetic disorder that gradually deteriorates a person’s physical and mental abilities. In the 1990s, the center began to store the brains of those with Parkinson’s and other neurodegenerative diseases. The center’s collection grew even more when it fused with the work of the National Institute on Aging’s Baltimore Longitudinal Study of Aging. The BRC performs the neuropathology for all the study participants who are autopsied. “It’s safe to say without the support of the National Institute on Aging, there is no brain bank here today,” says Troncoso, a native of Chile who emigrated to the United States in the 1970s to study pathology.
The center moved to its current location in the early 1990s. Today, the Johns Hopkins Brain Resource Center is one of dozens of brain banks across the country, with most having a particular focus or specialty. The VA Biorepository Brain Bank in Los Angeles, for example, specializes in amyotrophic lateral sclerosis, known as ALS or Lou Gehrig’s disease. The Mayo Clinic Brain Bank in Florida, like the BRC, focuses on Alzheimer’s disease, Parkinson’s disease, ALS, and stroke. The National Institutes of Health funds the NeuroBioBank, a network of six sites including one at the University of Maryland that specializes in developmental disorders.
Troncoso says an important role of a brain bank is that in addition to the physical collection, you have a detailed characterization of each brain’s morphology—its structure and changes over time—coupled with good clinical information gathered during the donor’s life. In a sense, researchers get to see the before, during, and after of a disease. Troncoso gives the example of Alzheimer’s disease progression, which we now know—thanks in part to brains at the BRC and similar brain banks—starts fairly early, in a person’s 40s, but manifests later in life.
“That’s important to know because although we’ve worked on a lot of treatments for Alzheimer’s disease, nothing really works yet,” Troncoso says. “Part of the reason why is that they’re tried in people who are too advanced. There’s nothing we can do. But what if we caught it early and could somehow stop these proteins from getting stuck in someone’s brain?”
Most people are not necessarily eager to donate their brains. If you’re an organ donor, that typically means your heart, corneas, and kidneys might go to someone, but the brain will not unless you’ve made separate arrangements to donate it. When participants join the Baltimore Longitudinal Study of Aging, or clinical studies at Johns Hopkins Alzheimer’s Disease Research Center, they are asked whether they would like to become a donor, giving their brain to be autopsied and used for research.
If they say yes, that’s where Karen Fisher, the center’s autopsy coordinator, enters the picture. Fisher is the center’s main conduit with the donor and his or her family. She passes on all the relevant information, including how to alert the center at the time of death. The approval is not binding, however, as by Maryland law the next of kin needs to authorize donation after a person dies.
Many consent, but some don’t, owing to religious prohibitions or concerns that brain removal may cause disfiguring that would be noticeable in an open casket viewing. The center’s staff assure them that will not be the case, as the brain is removed through an incision in the back of the head. Nobody would know the difference.
When someone dies, time is of the essence in terms of brain donation. Pathologists need to collect the brain promptly, typically within 24 hours of death to preserve biochemistry. The next of kin will alert the center and the funeral home, which arranges to transport the body to Johns Hopkins Hospital for an autopsy. For those out of state, the BRC will often work with the local hospitals and pathologists. If a patient dies in Houston, for example, no problem. All the autopsy information on Alzheimer’s patients, no matter where the procedure is performed, is submitted to the National Alzheimer’s Coordinating Center, which was established in 1999 by the National Institute on Aging to facilitate collaborative research.
Olga Pletnikova, a Moscow-born research associate in the Department of Pathology and manager of the Brain Resource Center, is primarily responsible for the removal and preparation of donated tissue, and distributing pieces of the collection to researchers and collaborators at Hopkins and other universities.
At the autopsy, a pathologist performs a complete physical examination of the person, recording details like skin color and body marks, before the brain is harvested out of the skull, weighed, and placed on dry ice for transport to the BRC. Once the brain arrives at the center, Pletnikova, or a neuropathology fellow, will carry out a complete macroscopic examination of the brain, noting marks and all physical characteristics. They look to see whether the brain appears normal, has plaques, has lesions, or shows any signs of atrophy. All observations are recorded in the database.
“Our collection really is the final step in the study of patients that clinicians and researchers have been tracking for, in some cases, many years,” Pletnikova says. “We are very thorough.”
Following the gross examination, the brain is prepared for storage. Using a scalpel, a trained pathologist will carefully separate the brain’s two hemispheres. “Of course, you don’t want to damage the tissue. And you never know what could happen, as at this point we don’t have the full diagnosis,” she says. “The person can have other diseases, such as mad cow disease or hepatitis. So we’re very conscious of contamination.”
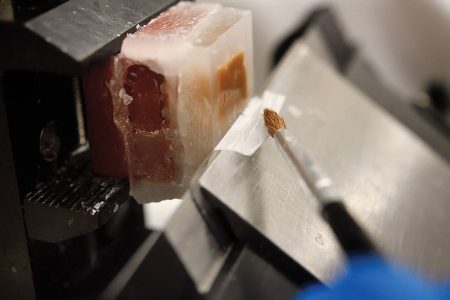
Following the separation, one hemisphere is placed in a plastic container filled with formalin, a solution of water and formaldehyde that serves as an antiseptic, disinfectant, and fixative. Here in the bath, the brain will harden so it can later be dehydrated, cut into sections, and then embedded in paraffin wax blocks that can be sliced microthin—down to 10 microns—on precision machines. Pieces of the brain are sent to the center’s lab to confirm diagnosis.
The other hemisphere is fast frozen using methyl butane and dry ice, and then placed in freezers where it is kept at -80 degrees Celsius—give or take a degree—to minimize decay. These frozen tissues, which can stay safe in storage for decades, are mostly used for biochemical, molecular, and genetic studies. Each freezer, which can hold roughly 100 samples, has an alarm that goes off if, for any reason, the temperature falls outside the accepted range. Troncoso says that losing power—and having the backup generators fail—is one thought that keeps him up at night. “As you can imagine, these brains are very valuable to us,” he says. “We need to keep them stable to preserve their biochemistry and appearance.”
he BRC works primarily with the research community for the specific neurologic diseases represented in its collection. First in line are faculty at Johns Hopkins, but there are 30 Alzheimer’s centers across the country, and they know where to go when searching for tissue samples.
The BRC generally doesn’t deal with nonacademic institutions, and sometimes a request is denied because there is only so much left of a portion of someone’s brain. The substantia nigra, for example, is a basal ganglia structure located in the midbrain that plays an important role in movement and the release of dopamine, and it is roughly the size of a thumbnail. Since Parkinson’s disease involves the decrease of dopamine production, researchers are keen to study this part of the brain to uncover what mechanisms are failing and why. The hippocampus is the most often requested brain region for those studying Alzheimer’s.
I might tell people I can’t give you this part, but I have plenty of frontal cortex samples,” he says. “Our cases are very valuable, and we try to share them with people who we know are going to do great work with it.” A standard request might be a researcher looking for eight to 10 Alzheimer’s cases with a certain degree of severity and tissue slices from this region and frozen samples from another. Most donors suffered from more than one disease, Troncoso says. A person can have dementia and also Parkinson’s and signs of strokes. “I’ll ask them, do you mind if they have something else? It’s important before you give out the tissue to let the researcher know exactly what they’re getting, and that is why it’s so important you have a good characterization of those tissues.” And they’ll often ask for some control brains, relatively disease-free brains that can be used for contrast.