 The cytotechnologist is one of the newer allied health professionals in medicine, far younger than either the medical technologist or histotechnologist. In the early 1950s, Dr. George Papanicolaou made a discovery that would change the face of cervical cancer detection. As with many ground-breaking discoveries, it was made by accident. Dr. “Pap” was studying the estrous cycle of the female when he noticed abnormally sized and shaped cells which he had scraped from the cervices of some of his subjects. These patients either currently had, or soon developed squamous carcinoma of the cervix. By convincing the medical community of the importance of his discovery, the “Pap smear” was born.
The cytotechnologist is one of the newer allied health professionals in medicine, far younger than either the medical technologist or histotechnologist. In the early 1950s, Dr. George Papanicolaou made a discovery that would change the face of cervical cancer detection. As with many ground-breaking discoveries, it was made by accident. Dr. “Pap” was studying the estrous cycle of the female when he noticed abnormally sized and shaped cells which he had scraped from the cervices of some of his subjects. These patients either currently had, or soon developed squamous carcinoma of the cervix. By convincing the medical community of the importance of his discovery, the “Pap smear” was born.
 In order to provide this test to patients, it became necessary to develop a workforce trained in cancer detection. The infant field of cytotechnology was born in the gynecologist’s office. By showing other allied health professionals how to stain smeared slides and the subtle nuances of abnormal epithelial cells, the field became a pivotal adjunct to women’s health. It became the responsibility of the cytotechnologist to microscopically examine all of the cells on the slide – anywhere from 50,000 to 500,000 on each slide. The cells of interest were marked for the pathologist. As the popularity of the Pap smear grew, the premise of examining human cells for cancer and its precursors was taken up in areas other than gynecology. Spontaneously exfoliated cells in sputum and urine were easily obtainable from patients who might harbor malignancies. Consequently the discipline of cytopathology and the cytotechnologist branched out into the respiratory and urinary arenas. By this time, formal training in specialized schools of cytotechnology was required of the practitioner, and the Johns Hopkins Hospital helped to lead the way. Dr. John Frost, a JHH cytopathologist and Director of Cytopathology from 1959 to 1989, established one of the earliest schools of cytotechnology in the United States. Now requiring at least a bachelor’s degree with a concentration in biological sciences, this 12-month program graduated students ready to sit for the American Society for Clinical Pathology examination.
In order to provide this test to patients, it became necessary to develop a workforce trained in cancer detection. The infant field of cytotechnology was born in the gynecologist’s office. By showing other allied health professionals how to stain smeared slides and the subtle nuances of abnormal epithelial cells, the field became a pivotal adjunct to women’s health. It became the responsibility of the cytotechnologist to microscopically examine all of the cells on the slide – anywhere from 50,000 to 500,000 on each slide. The cells of interest were marked for the pathologist. As the popularity of the Pap smear grew, the premise of examining human cells for cancer and its precursors was taken up in areas other than gynecology. Spontaneously exfoliated cells in sputum and urine were easily obtainable from patients who might harbor malignancies. Consequently the discipline of cytopathology and the cytotechnologist branched out into the respiratory and urinary arenas. By this time, formal training in specialized schools of cytotechnology was required of the practitioner, and the Johns Hopkins Hospital helped to lead the way. Dr. John Frost, a JHH cytopathologist and Director of Cytopathology from 1959 to 1989, established one of the earliest schools of cytotechnology in the United States. Now requiring at least a bachelor’s degree with a concentration in biological sciences, this 12-month program graduated students ready to sit for the American Society for Clinical Pathology examination.
As time went on, the endoscope, a flexible snake-like instrument used by radiologists to peer into the major bronchi among other areas, catapulted the entire discipline of cytopathology into the forefront of cancer detection. Through the endoscope, suspected areas of concern could be scraped or washed, thus saving the patient an open biopsy. These techniques worked for lesions that were either originally on the surface or had eroded through the epithelium and thus communicated with the surface. Soon there was another technique, fine needle aspiration, on the horizon, and the cytotechnologist was about to meet patients for the first time.
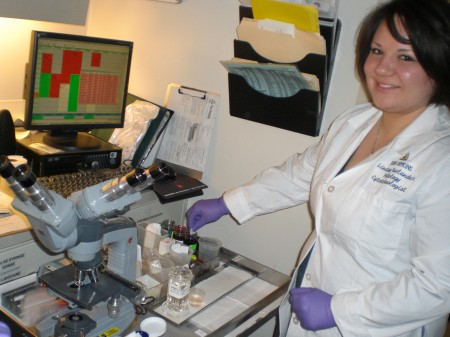
Fine needle aspiration (FNA) involves the insertion of a very thin bore needle, thinner than that used in phlebotomy, into an identified abnormality in order to obtain a diagnosis. This can be done for superficial lesions as well as those which are deep inside the body. This technique is safe, cost-effective, and efficient. In an expanded role, the cytotechnologist can enhance the efficiency of the procedure by being in attendance when the aspiration is performed. Although cytopathologists are often involved in this evaluation process, because there is more demand for FNA assessment than hours in the day for the cytopathologist, the cytotechnologist has been called to perform part of the assessment process. Cytotechs guide the clinician to the right area of the lesion to sample. By performing a “pass” into the area of concern, aspirating some cells, withdrawing the needle and allowing the cytotechnologist to stain and examine those cells, the efficiency of the entire FNA can be increased. If diagnostic cells are not present, the procedure can be repeated, several times if necessary.
The cytotechnologist cannot give a diagnosis, as that privilege is reserved for the cytopathologist. Even so, the cytotech has evolved into someone who, in addition to the more routine work of Paps and medical cases, can often be seen pushing the aspiration cart, including the microscope and stains, into the endoscopy suite in Carnegie. When the new Clinical Building opens, although the Division of Cytopathology itself will not move, there will be ancillary space adjacent to the ultrasound rooms on the second floor. The procedure rooms will increase extensively and the cytotech cadre will be busier than ever. Use of new molecular techniques will require the cytotechnologist to further refine the specimen collection technique as the field looks forward to a bright future!
Fran Burroughs, SCT(ASCP)IAC
Supervisor, Cytopathology Technical Operations
Department of Pathology