 The Department of Pathology, in collaboration with the Office of Innovations, Central Information Technology, and JHH Nursing, has been working very hard in both the search for and the financial approval of a new barcode point-of-care system (BPOC). In the past year we completed extensive reviews and site visits and eventually selected the CareFusion® BPOC for the Hospital. The catalyst for this search was galvanized by a sentinel event in which a patient was misidentified prior to having a type and cross-specimen collected. The ultimate result was the patient received two units of the wrong type of blood. This event, in addition to an array of regulatory concerns, helped solidify the support needed to implement this solution to all inpatient units. This barcode technology has been successfully demonstrated at other medical facilities and has eliminated many of the issues that currently impact our Laboratory operation. The hospital will initially contract for two modules:
The Department of Pathology, in collaboration with the Office of Innovations, Central Information Technology, and JHH Nursing, has been working very hard in both the search for and the financial approval of a new barcode point-of-care system (BPOC). In the past year we completed extensive reviews and site visits and eventually selected the CareFusion® BPOC for the Hospital. The catalyst for this search was galvanized by a sentinel event in which a patient was misidentified prior to having a type and cross-specimen collected. The ultimate result was the patient received two units of the wrong type of blood. This event, in addition to an array of regulatory concerns, helped solidify the support needed to implement this solution to all inpatient units. This barcode technology has been successfully demonstrated at other medical facilities and has eliminated many of the issues that currently impact our Laboratory operation. The hospital will initially contract for two modules:
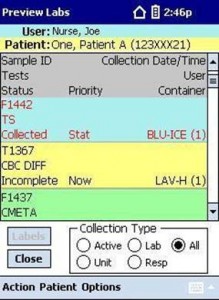
 The Specimen Collection Application will support the clinicians’ need to integrate bedside specimen collection and labeling of specimens to positively identify the patient. Currently, JHH phlebotomists are using a “homegrown” BPOC application that uses pre-generated specimen labels. Our PDS solution has also been deployed in the Emergency Department where dramatic decreases in specimen collection defects have been noted. The new application has additional operational features and will be deployed in four phases:
The Specimen Collection Application will support the clinicians’ need to integrate bedside specimen collection and labeling of specimens to positively identify the patient. Currently, JHH phlebotomists are using a “homegrown” BPOC application that uses pre-generated specimen labels. Our PDS solution has also been deployed in the Emergency Department where dramatic decreases in specimen collection defects have been noted. The new application has additional operational features and will be deployed in four phases:
1. Core Lab Phlebotomy
2. Emergency Department and Vascular Access Phlebotomy
3. Intensive Care Units and Oncology
4. General Wards, Pre- and Post-Op Surgery
By the spring of 2010, we hope to be fully deployed on all 70 inpatient units.
An overview of the steps to use the system include:
1. Obtain a handheld device and wireless printer from the charger.
2. Log-on onto the handheld device with your ID and password.
3. Scan the patient’s barcode wristband.
4. Review the patient orders (Lab, Nurse, or VAT) collections.
5. Select the desired orders for collection at this session.
6. Press “Print” to generate specimen label printing at the patient’s bedside.
7. Collect the requested blood, urine, fluid, and/or culture specimens.
8. Scan the collected specimen(s) to enter the current collection date/time.
9. Scan the patient’s wristband to close the collection encounter.
10. The handheld will direct the provider to the next patient.
 Regulatory and operational issues that will be addressed with this solution include:
Regulatory and operational issues that will be addressed with this solution include:
1. Identification of the specimen collector (no more “Background Job”).
2. Accurate collection date and time at the patient’s bedside.
3. Eliminate the lab receipt of cancelled specimens (no pre-printed labels).
4. Process for the collection of specimen related information (dosage, etc).
5. Eliminate the ICU issue with multiple labels and one tube. By printing at the last minute, all orders can be aggregated into the least amount of specimen tubes.
6. Eliminate the possible use of pre-printed specimen labels on the wrong patient.
7. Scan of patient wristband at the end forces closure of session at the bedside.
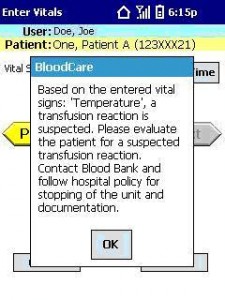
 The other module that will begin deployment in July 2010 is Barcode Transfusion Verification. This application will support our efforts to comply with the National Patient Safety Goals, “Improve the accuracy of patient identification” and “Eliminate transfusion errors related to patient misidentification.” The NPSG specifically referenced barcode technology as a sufficient replacement if two individuals are not available to verify patient identity. The implementation of this module should consistently provide the required transfusion-related information to comply with AABB and CAP regulations. This includes documentation of the provider who administered the blood product; the identification of the individual who witnessed the process; the exact start time of the infusion; the end time of the transfusion; and the documentation of baseline and 15-minute patient vitals. All of this information is collected through the CareFusion® software process, either by a handheld device or a computer on wheels (COW). The system automatically alerts the provider if an entered vital sign is out of an acceptable range and also triggers the information flow if a transfusion reaction work-up is required. The end product is a fully documented in a “Transfusion Verification Report” that can be customized to meet the specific needs of our Institution. This report can be printed for insertion into the patient chart, imported into the Blood Bank, and imported into the Patient EMR. Completion of this data will allow Transfusion Medicine to track the outcomes of all transfusions and close the loop on missing regulatory data.
The other module that will begin deployment in July 2010 is Barcode Transfusion Verification. This application will support our efforts to comply with the National Patient Safety Goals, “Improve the accuracy of patient identification” and “Eliminate transfusion errors related to patient misidentification.” The NPSG specifically referenced barcode technology as a sufficient replacement if two individuals are not available to verify patient identity. The implementation of this module should consistently provide the required transfusion-related information to comply with AABB and CAP regulations. This includes documentation of the provider who administered the blood product; the identification of the individual who witnessed the process; the exact start time of the infusion; the end time of the transfusion; and the documentation of baseline and 15-minute patient vitals. All of this information is collected through the CareFusion® software process, either by a handheld device or a computer on wheels (COW). The system automatically alerts the provider if an entered vital sign is out of an acceptable range and also triggers the information flow if a transfusion reaction work-up is required. The end product is a fully documented in a “Transfusion Verification Report” that can be customized to meet the specific needs of our Institution. This report can be printed for insertion into the patient chart, imported into the Blood Bank, and imported into the Patient EMR. Completion of this data will allow Transfusion Medicine to track the outcomes of all transfusions and close the loop on missing regulatory data.
 The implementation of these two modules will forever change many of the challenges that our Laboratory currently faces. We hope to eliminate much of the “confusion” with our current specimen collection processes. By having all collectors using the same process, we will all be able to view the patients across the various services and hopefully eliminate multiple phlebotomy sticks to the patient. We should see a dramatic reduction in the receipt of uncollected specimens, cancelled specimens, and misidentified specimens. This product has been successfully installed all of the VA hospitals and at many hospitals throughout the United States. We are very hopeful that CareFusion® BOPC will also be successfully implemented at Johns Hopkins Hospital. Give the project scope and the complexity of our Institution, it will be an exciting time to be part of this process.
The implementation of these two modules will forever change many of the challenges that our Laboratory currently faces. We hope to eliminate much of the “confusion” with our current specimen collection processes. By having all collectors using the same process, we will all be able to view the patients across the various services and hopefully eliminate multiple phlebotomy sticks to the patient. We should see a dramatic reduction in the receipt of uncollected specimens, cancelled specimens, and misidentified specimens. This product has been successfully installed all of the VA hospitals and at many hospitals throughout the United States. We are very hopeful that CareFusion® BOPC will also be successfully implemented at Johns Hopkins Hospital. Give the project scope and the complexity of our Institution, it will be an exciting time to be part of this process.
Mike Huppenthal
Systems Integration Manager
Johns Hopkins Medical Laboratories
