How the H1N1 Virus Changed the Face of Respiratory Virology Testing
The traditional respiratory virus season is principally during the colder winter months, typically October through March. During this time, the predominant respiratory viruses seen are respiratory syncytial virus (RSV) and influenza A or B. Throughout the year, we see additional respiratory viruses such as adenoviruses, enteroviruses, parainfluenza virus types 1-4, human metapneumovirus (hMPV), and rhinoviruses. RSV is the major cause of lower respiratory tract infection and hospital visits for young children. Influenza A and influenza B, also called seasonal flu, result in 36,000 deaths and more than 200,000 hospitalizations nationwide each year. The annual cost in the United States for influenza is estimated to be greater than $10 billion. Adenoviruses, enteroviruses, parainfluenza viruses, rhinoviruses, and hMPV can be severe in some patient populations, but most patients are not hospitalized.

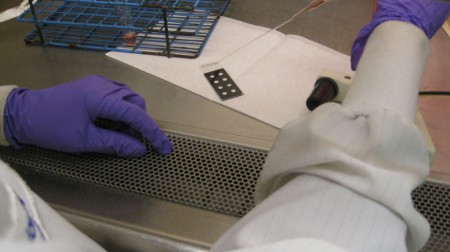
Processing respiratory viral samples for testing
A variety of methods can be used to diagnose these viral infections in the Laboratory. Ultra-rapid (15-minute) antigen detection assays that are similar to over-the-counter pregnancy tests are available for influenza A, influenza B and RSV. Virus antigens can also be found by staining cells obtained from patient specimens with fluorescent-tagged anti-viral antibodies and examining stained preparations using a fluorescence microscope. This method is known as the direct fluorescent antibody (DFA) test and it can be used to detect RSV, influenza A/B, parainfluenza virus types 1-3, adenoviruses, and hMPV. Before the availability of sophisticated molecular tests such as PCR, viruses were amplified and detected the old-fashioned way, by culturing specimens in cells. Two types of culture are available: rapid (48-hour) culture, known as “shell vial” (SV), and the conventional tube culture that can take up to three weeks. In the shell vial method, cells are grown on a coverslip that is placed in a small vial containing nutritive medium. The patient specimen is placed in the medium. The vial is then centrifuged and placed in an incubator. After 48 hours, the coverslip is removed from the vial and stained with fluorescently-tagged antiviral antibodies. Tube cultures consist of cells that are placed in a single layer along the side of a glass test tube. The tubes also contain nutritive medium that allows the cells to remain alive in culture. The patient specimen is placed into the tube and the cultures are incubated for up to three weeks. Virus is detected by examining the cells for changes in appearance that signal virus growth, termed “cytopathic effect.” Different viruses produce different cytopathic effects. Technologists are trained to identify these specific effects while examining cultures using light microscopes. Analysis of JHH Clinical Virology Laboratory data indicates that 55% of infections are detectable by DFA. An additional 35% of the respiratory viruses may be detected by the SV technique. The remaining 10% are detected by tube culture.

Reading tissue culture tubes under the inverted microscope
This past spring, a new influenza virus was found in patients with respiratory infections in Mexico and in two unrelated individuals in southern California. It was termed “Swine Flu” because its genetic material was found to be highly related to influenza strains that were grown from pigs. This novel virus did not act like typical seasonal influenza virus. It was occurring in warm weather months, it was spreading rapidly in school-aged children, and it was causing disease around the globe, eventually leading the World Health Organization to declare that the infection had become a pandemic.
Public anxiety grew over a rapidly advancing virus whose lethality was largely unknown, but increasingly feared, as Mexico was reporting high death rates. Here in the U.S., the healthcare system was flooded with alarmed patients complaining of respiratory symptoms. At JHH, plans that had been formulated to deal with a potential avian influenza outbreak were activated to cope with the large patient influx and to prepare for a potentially lethal pandemic. The JHH Clinical Virology Laboratory was inundated with requests for respiratory virus testing. Typically, the month of May is the beginning of the slow season for respiratory viruses and the Laboratory would normally process about 200 respiratory specimens. In May 2009, well over 1,000 of these samples arrived for testing.
There was a silver lining to a workload that was so large that it drained resources and strained staffing, as it served as a catalyst for change. Respiratory virus algorithms employing the full range of conventional tests were clearly no longer practical. Although the Laboratory has shown that its algorithm is comparable in performance to highly sensitive molecular methods for viruses such as RSV and influenza A & B, the labor required to achieve this result was tremendous and unsustainable. In addition, patient results were frequently delayed due to the time required to recover viruses in tube cultures. In response and after extensive consultation with clinical colleagues, the staff in the Medical Microbiology Division has formulated a new set of respiratory virus algorithms that should offer sensitive detection, speedy diagnosis, and greatly streamlined workflow.
Beginning on November 2, 2009, at 11:00 a.m., the face of respiratory virus testing will change at JHH. Two different respiratory virus detection panels, one for standard patients, and one for immunocompromised patients will be offered. Care providers will be asked to provide the category that qualifies a patient for the immunocompromised panel (see Table below for Immunocompromised Panel Qualifying Categories). The initial test in both panels will be the DFA test, the gold standard in rapid time-to-result respiratory virus tests. If DFA is positive, the virus will be reported and no further testing will be performed. If the DFA is negative, shell vial culture will be performed for standard patients, and multiplex PCR will be performed for immunocompromised patients. The multiplex PCR will detect 10 respiratory viruses (RSV, influenza A, influenza B, parainfluenza virus types 1-4, hMPV, adenoviruses, and rhinoviruses). All respiratory virus test results should be finalized 48 hours after a specimen arrives in the Laboratory. In addition, the Clinical Virology Laboratory will now also accept nasopharyngeal swabs collected with a Flocked Swab (SAP #114949) for both respiratory virus panels. Ultra-rapid antigen detection assays and tube cultures for respiratory viruses will be discontinued.

Multiplex PCR instrumentation
These changes will have many advantages. Improvements that should be obvious to patients and care providers include decreased time-to-result and more effective detection of certain viruses such as hMPV and rhinoviruses by PCR. Compared to nasopharyngeal aspirates, nasopharyngeal swabs should be easier to collect by the provider and more comfortable for patients. Swabs also minimize the potential for aerosolizing virus, eliminating the need for specialized collection environments. From the Laboratory’s perspective, overall efficiency will improve due to workflow changes and eliminating tube inoculation and daily inspection. These gains will allow DFAs to be performed 24/7 for the first time, with a time-to-result of up to 4 hours. Swabs, which have less mucus than aspirates, will also be beneficial to the Laboratory as they are easier to process and result in fewer uninterpretable DFAs.
Additional information on swab collection and the new respiratory virus test panels can be found on the JHH Medical Microbiology web site.
| Immunocompromised Panel Qualifying Categories |
| Oncology |
| Solid Organ Transplant |
| ICU |
| Neonate |
| HIV |
| Receiving Immunomodulator Therapy |
| Pregnant |
| Normal host, sudden onset respiratory failure |
Ame’ Maters
Supervisor, Medical Microbiology Laboratory
Alexandra Valsamakis, M.D., Ph.D.
Director of Clinical Virology and Molecular Microbiology
Associate Professor of Pathology

I understand your article that you can test faster for H1N1 but it doesn’t really matter when doctors are all over the place with their solutions. I have H1N1 right now, and my doctor said yesterday I am not a candidate for tamiflu because I don’t have underlying causes like asthma. My 4 year old and 1 year old can’t get the drug either. I called my ped. and she said since the 1 year old had rsv and bronchiolitis last year, if her fever is over 103 bring her in and we’ll consider tamiflu. But what about the 4 year old- when she’s sick it goes into her lungs, I have bottles of albuterol to prove it. Both girls are sick today with 102 fever and the 4 year old has aches. But I am not bringing them in to the doctor and am so worried that they are going to have to go to a hospital in the next few days because when they get sick its in their lungs. This in in VA. In MD, my friend’s son has H1N1 and they gave him tamiflu and he does not have asthma and they gave the mother tamiflu even though she has no symptoms. That’s right- no symptoms = tamiflu in MD while actually being sick = no tamiflu here. In Denver, my brotherinlaw had H1N1 and they gave him tamiflu- he’s asthmatic and he got pnomonia and they prescribed leviquen even though there is a law suit against that drug currently. The doctor said if you want something different go to a hospital. It’s been 14 days. So the answer is who knows.
Thanks for posting this, I found it very informative.