In June of 2006, the FDA notified health care professionals and the public about the risks and factors that linked gadolinium-based contrast media to nephrogenic systemic fibrosis (NSF) in patients with impaired renal function. Because of the risks, it is critical to assess the patient’s renal function prior to administration of this contrast.
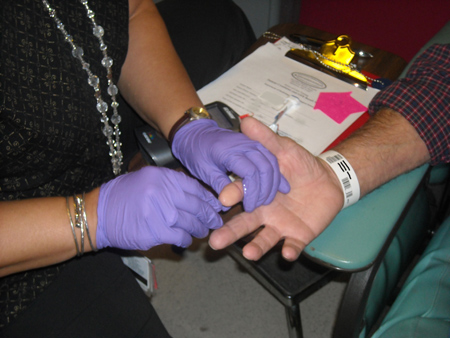
MRI tech doing a fingerstick on a patient in JHOC.
Prior to January 2008, our patients at Hopkins had to get their blood drawn either prior to coming for their MRI or have it drawn when they got here. If it was done the same day of the procedure, the patient had to go to Express Testing in JHOC to get their blood drawn and then wait for the results from the Lab, which can take up to an hour. The logistics of this process were inconvenient. Having patients scheduled to have their MRI in Nelson and their blood drawn in JHOC presented challenges for the elderly patients who would have to travel back and forth between buildings. Thus, this also became a patient satisfaction issue.
It was then that the Point-of-Care Testing Office (POCT) received requests to have Creatinine testing available at the MRI sites. Our office evaluated several meters and decided to purchase the Nova StatSensor. We implemented the first meters in Nelson and JHOC MRI, and now have seven sites and about 40 operators certified to do testing.
With the Creatinine Point-of-Care device, renal function is assessed with a fingerstick and it takes approximately 20 seconds to get an answer. It can then be determined if the patient should be getting a full dose of the contrast or none at all.
As part of our continuous Quality Assurance monitoring, we added these new Creatinine testing sites to our daily rounds. We visit all the locations and review the QC and patients who have been tested on the meter. Our office is also responsible for monitoring correlations with the Core Lab on a monthly basis, and investigating reasons for discrepant results.
MRI tech applies the blood to the strip
Daily rounds also give us an opportunity to interact with the end-users and sometimes the patients who find that getting the testing done right then and there and getting an answer right away is much better than waiting around.
“It makes a huge difference to the patient. They really like the idea of having it done much quicker,” says Melody Corbin from JHOC MRI. “It’s nice that they don’t have to go to the Lab. It’s an easy and quick thing to do. We need more people trained to do it!” says Bill White also from JHOC MRI.
Carol Lonsdale RT, R MR CT, highlights how the testing process has actually changed. Before having POC Creatinine available, the patient had to go to the Lab and get drawn. As they waited for results, sometimes they would bring the patient in the MRI room and do the pre-contrast testing. When the Lab results were available, they would bring the patient back in and finish with the post-contrast imaging. “This was very inconvenient for the patient and it would also throw off our schedule. We were late for the appointments and the patients just had to wait around too long. This way is so much more convenient,” Carol said.
Implementation of Creatinine POC testing has helped improve the workflow for the MRI areas by giving them a fast and much more convenient way of assessing the patient’s renal function prior to applying contrast. We also feel that patient satisfaction has improved significantly and after all, that’s what we are here for.
Point of Care Coordinators. From left to right, Karen Reilly, Leandra Soto, Lois Phelan. Not pictured, Sandy Humbertson.
Leandra Soto, MT(ASCP)
Lois Phelan, MT (ASCP)
Karen Reilly, MT (ASCP)
Sandy Humbertson, MT (ASCP)
Johns Hopkins Point-of-Care Office